Every time I watch the news or read some article there’s always conflicting information regarding which time is the best time to get some sunlight and which sun rays are more harmful. That’s why I decide to bunker down and do some serious research so I can really understand the sun’s ray and our health. Here’s what I learned!
*Warning: This blog post is VERY LONG since I want to include as much information as I can to help you understand the whole picture. Snacks and bathroom break are recommended! Please read till the end and you won’t regret it 🙂 *
You ready?
Let’s begin!
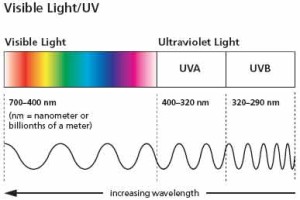
Ultraviolet (UV) radiation is part of the light spectrum that reaches the earth from the sun. You cannot see these light since its wavelengths are shorter than visible light. These wavelengths are UVA, UVB, and UVC.
UVA is the longest: 320-400 nm (billionths of a meter) account for about 94% of the radiation. There are two forms of UVA:
UVA1 (longwave UVA) 340-400nm
UVA2 (shortwave UVA) 320-340 nm
UVB ranges from 290-320 nm account for about 5% of radiation
UVC is the shortest (100-290 nm) and doesn’t reach the earth; account for about 1%, it is absorbed by the ozone layer.
Both UVA and UVB can penetrate the ozone layer and can cause lot of skin and health problems.
Both the U.S. Department of Health and Human Services and the WHO have identified UV as a proven human carcinogen. UV ray can produce genetic mutations by alter skin’s cellular DNA leading to skin cancer. UV radiation is considered the main cause of nonmelanoma skin cancers (NMSC), including basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). Many experts also believe that UV radiation also play a key role in melanoma, the deadliest form of skin. cancer.
UVA
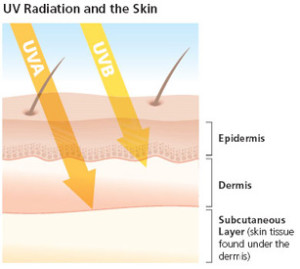
UVA rays account for up to 94% of the UV radiation reaching the Earth’s surface. They are less intense than UVB but are 30 to 50 times more prevalent. They are present with relatively equal intensity during all daylight hours throughout the year and can penetrate clouds and glass.
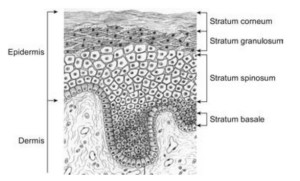
UVA rays are mostly responsible for the generation of reactive oxygen species (ROS) leading to oxidative stress. It can penetrates the skin more deeply than UVB into the deep dermis and induce dermal damage. It is not absorbed directly by the DNA of the keratinocytes but can damage the cells through oxidative stress.
A mini review: The keratinocytes are form by mitosis and as they matures they move outward from the basal layer and shed on the skin surface. …..to learn more just hop back to this post.
What are ROS?
Reactive oxygen species (ROS) are chemically reactive molecules containing oxygen. ROS are formed as a natural byproduct of the normal metabolism of oxygen and have important roles in cell signaling and homeostasis. However, during times of environmental stress (e.g., UV or heat exposure), ROS levels can increase dramatically. This may result in significant damage to cell structures. Cumulatively, this is known as oxidative stress.
In general, harmful effects of reactive oxygen species on the cell are most often:
- damage of DNA
- oxidations of polyunsaturated fatty acids in lipids (lipid peroxidation)
- oxidations of amino acids in proteins
- oxidatively deactivate specific enzymes by oxidation of co-factors
https://en.wikipedia.org/wiki/
Basically you don’t want your level of ROS to increase because it will cause lot of bad reaction in your body. It will signal your body to react negatively. ROS and inflammation are the root of all disease in my opinion!
In these studies, to induce ROS on reconstructed skin they exposed the skin to different doses of UVA1 (ranging from 10 J/cm2 to 40 J/cm2) and compared the results.
- They found the increase in ROS production in both dermal fibroblast and epidermal keratinocytes is depend on the dose of UVA1 exposure. It can be detect starting at a dose as low as 10 J/cm2 UVA1. At this dose ROS were detected up to 188 mm deep in dermis and reached the deepest cells of the dermis at 30 and 40 J/cm2 UVA1. Keep in mind that the skin thickness is range from 0.3-4mm depending on the location. Exposure to 40 J/cm2 UVA1 can alter gene expression in both fibroblasts and keratinocytes of reconstructed skin.
(source: http://www.
- 8-isoprostane, a derivative of arachidonic, is an established marker for lipid peroxidation. It’s found to be dose-dependent increase in the culture medium of reconstructed skin exposed to UVA1. It can increase to 9 times for the 40J/cm2 UVA1 dose, as compared to unexposed sample.
- Cyclobutane pyrimidine dimer (CPD) was also detected in the reconstructed skins after exposing to UVA1. CPD is one of UV products. It is premutagenic lesion and can alter the DNA structure. Our body can repair this by photo reactivation or nucleotide excision but unrepaired are mutagenic and can cause cancer.
UV can induce immunosuppression and pro-inflammatory. Since UVA1 is more prevalent in solar UV, their relative solar immune suppressive efficiency is about threefold higher than that of UVB at doses received during normal daily activities.
The maximal doses of UVA1 used in the study was 40 J/cm2 corresponding to a physiological dose that could be received in a few hours. The study showed that many of the biological changes induced by UVA1 occurred at much lower dose than 40 J/cm2.
So what does J/cm2 means? How does it compare in terms of sunlight hours?
10 J/cm2 UVA is equivalent to 1 hour of exposure midday in June. So if you spend 4 hours in the sun you probably will receives the maximum doses of 40 J/cm2 similar to the study.
Do you like tanning bed? I got bad news for you…
UVA is the dominant tanning ray. The high-pressure sunlamps used in tanning salons emit doses of UVA as much as 12 times that of the sun. People who use tanning salons are 2.5 times more likely to develop squamous cell carcinoma, and 1.5 times more likely to develop basal cell carcinoma. International Agency for Research on Cancer has considered tanning lamps as carcinogenic. The risk of developing a melanoma is increased by 75% in those who regularly use tanning lamps up to the age of 30. Yikesss!
Studies in mice also showed that UVA1 were carcinogenic and responsible for photo-aging signs such as dryness, skin thickening, leathery appearance, sagging and wrinkling. In humans, UVA1 exposure during phototherapy sessions leads to acute side effects including skin dryness, pruritus, polymorphic light eruptions and herpes simplex virus reactivation.
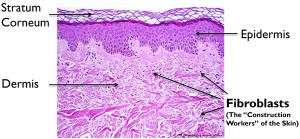
Experiments with reconstructed skin show that UVA1 induced fibroblasts death by induction of apoptosis six hours after exposure to UVA1.
- Fibroblasts: are cells in connective tissue (deep inside the dermis that produces collagens and fibers.
- Apoptosis: programmed cell death.
The epidermis wasn’t effect to that extent only some alteration of granular layers when expose to UVA1. Induction of apoptosis was not detected.
(source: http://www.
(Source: the handbook of cosmetology)
phew! we got through UVA yay! let’s continue with UVB shall we?
UVB
UVB has been extensively studied. UVB can directly induce DNA damage and form potentially carcinogenic photoproducts. Only UVB are responsible for the production of Vitamin D by direct conversion of 7-dehydrocholesterol into vitamin D3. UVB is the chief cause of skin reddening and sunburn, tends to damage the skin’s more superficial epidermal layer. Its intensity varies by season, location, and time of day. The most significant amount of UVB hits the U.S. between 10 AM and 4 PM from April to October. UVB rays can burn and damage skin year round, especially at high altitudes and on reflective surfaces such as snow or ice, which bounce back up to 80 percent of the rays so that they hit the skin twice. UVB rays do not significantly penetrate glass.
Early morning and late afternoon, the sun ray are more oblique. As the sun become more oblique to the earth’s surface, the UVB photons have to travel a longer path to reach earth, the ozone which efficiently absorb them. Therefore most if not all of the UVB photon are absorbed by the ozone layer. In contradiction to this we have been repeatedly told to have some sunlight during this hour. What’s the point then? We wouldn’t be getting any vitamin D at that hour just the harmful UVA rays. No thank you! Keep reading and you will understand why we need some nature UVB 😉
Our major source of vitamin D comes from exposure to sunlight, UVB to be exact. And how does we know sunlight is good for us? What kind of health benefits does it provide? Let us travel back in history….
Vertebrates that evolved in the ocean lives in high calcium environment and they used it for developing a mineralized endoskeleton. When vertebrates ventured onto land, which is calcium poor environment, they adapt to it by increasing their efficiency for intestinal absorption of dietary calcium. They have the ability to photosynthesize vitamin D3 in their skin which became essential for enhancing intestinal calcium absorption and maintaining serum calcium levels in most land vertebrates including homosapiens.
Even in as early as 1600s physician has recognize that higher incidence of rickets in children happened in industrialize cities compare to children living in the countryside was due to lack of sun exposure and that ‘sunbathing’ was important for preventing rickets.
Rickets is a disease of children caused by vitamin D deficiency, characterized by imperfect calcification, softening, and distortion of the bones typically resulting in bow legs.
In 1903 Niels Ryberg Finsen received the Nobel Prize for his insightful observations that exposure to sunlight cured a variety of diseases including lupus vulgaris (skin infected with tuberculosis).
Very few foods naturally contain vitamin D. Those foods include oily fish (salmon, cod liver oil contains vitamin D3 and sun dried mushrooms contains vitamin D2). The major source of vitamin D (D2 or D3) for most humans is exposure to sunlight. Vitamin D3 is 2 to 3 times more effective in raising blood levels of 25(OH)D compared to the same dose of vitamin D2.
25(OH)D is Calcifediol (INN), also known as calcidiol, 25-
25(OH)D is mainly refer as total vitamin D.
Nowadays you see many foods is fortified with vitamin D. So is dietary vitamin D3 is the same as vitamin D3 made in the skin? Would consume fortified food be enough?
Typically there is 100 IU (10 mcg) of vitamin D in a serving (8oz) of milk or orange juice. Most of the time the fortified vitamin D add is vitamin D2. Although both type of vitamin D3 have the same biologic activity once they are metabolized in the body, the half-life of vitamin D3 produced in the skin is prolonged in the circulation because 100% is bound to the vitamin D binding protein whereas when vitamin D3 is ingested, only about 60% is bound to the vitamin D binding protein and 40% is rapidly cleared in the lipoprotein bound fraction.
Let’s talk about the vitamin D level that your physician usually order at your annual checkup.
1,25-dihydroxyvitamin D [1,25(OH)2D] is the biologically active form of the vitamin. Although 1,25(OH)2D is the active metabolite of vitamin D, serum levels of 1,25(OH)2D do not reflect the body’s stores and are not useful for determining vitamin D status. Doctors normally order this to differential diagnosis of hypocalcemia and to monitor patients with renal osteodystrophy or chronic renal failure. 1,25-dihydroxyvitamin D [1,25(OH)2D] is one of the most potent hormones for regulating cell growth and maturation. It is estimated that more than 200 genes are either directly or indirectly influenced by 1,25(OH)2D.
There are two main forms of vitamin D
– Vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol).
Vitamin D3 is the naturally occurring form of vitamin D in humans. It is made in the skin following exposure to sunlight (UVB). Vitamin D3 can also be found in certain fish and cod liver oil.
–Vitamin D2 is found in some vegetables, including mushrooms, and in many fortified foods (milk, yogurt, etc.).
Vitamin D tests generally measure the total concentration of 25(OH)D, (vitamin D3 + vitamin D2) which is the main form of vitamin D circulating in blood and the best indicator of vitamin D deficiency or excess. This is the test the doctor order when you go for your annually checkup. They can order just the vitamin D total or they can order the vitamin D total with the differentiation of 25(OH)D2 and 25(OH)D3. Thus, it is helpful for differentiating the contribution of prescription supplementation from sunlight and over-the-counter supplementation. This is because vitamin D2 is typically used in subscription formulations, vitamin D3 is the form produced subsequent to sun exposure, and vitamin D3 is more often used in over-the-counter supplements. Vitamin D2 is derived from fungal and plant sources and is commonly found in supplements, such as multivitamins, in the United States. Vitamin D2 may also be used in the pharmacological treatment of vitamin D deficiency.
Are you still with me??? Hang in there! We’re almost done 🙂
There have been numerous studies that have implicated living at higher latitudes and being at increased risk of vitamin D deficiency with many serious and chronic and deadly diseases including cancers of the colon, prostate and breast, autoimmune diseases including multiple sclerosis, type I diabetes and rheumatoid arthritis, infectious diseases including tuberculosis and influenza and hypertension and heart disease.
Exposure to sunlight results in an increase of circulating levels of 25(OH)D (this is the total vitamin D level) but not the bioactive form l,25(OH)2D. The reason is that parathyroid hormone, calcium and phosphorus and fiberblast growth factor 23 tightly control the production of l,25(OH)2D in the kidneys. 25(OH)D is incapable of altering vitamin D responsive gene expression at physiologic concentrations, but its bioactive form does. Many studies show that by increasing blood levels of total vitamin D level, our tissues and cells in the body will be able to produce locally the bioactive form l,25(OH)2D of vitamin D. The local production of 1,25(OH)2D is important for regulating cell growth and maturation and, thus, is able to prevent cells from becoming malignant. 1,25(OH)2D3 accomplishes this by either restoring the cell to its normal proliferative state or by inducing its death by apoptosis.
It is recommend that a 25(OH)D level (this is the total vitamin D) should be at least 30 ng/ml to have the full benefits of vitamin D for overall health. In order to attain a level above 30 ng/ml, 800 to 1,000 lU of vitamin D/day is required from dietary sources or from exposure to sunlight. Since diets that include vitamin D supplemented foods are only able to satisfy between 10 and 40% of this requirement, it is not at all surprising that vitamin D deficiency is probably one of the most common medical conditions world-wide.
The consequences of vitamin D deficiency are often silent, but insidious in nature. For children, it may prevent them from attaining their peak height and bone mineral density. Adults have an increased risk of developing osteopenia, osteoporosis and increase risk of fracture. In addition, vitamin D deficiency increases risk of a wide variety of chronic diseases.
What about sunlight and skin cancer?
Humans evolved in sunlight and our skin pigment gene has also evolved in order to protect our skin from the damaging effects from excessive exposure to sunlight, but at the same time permitting enough UVB radiation to enter the skin to produce an adequate amount of vitamin D to sustain health. During evolution our skin was designed to take advantage of the beneficial effect of sun exposure while minimizing the damaging effects.
The skin has a large capacity to make vitamin D3. When young and middle aged adults were exposed one time to one minimal erythemal dose (MED) of UVB, the circulating levels of vitamin D that were observed 24 hours after the exposure were similar to adults who ingested between 10,000 and 25,000 IU of vitamin D2. Thus only minimum exposure to sunlight is often adequate to satisfy the body’s vitamin D requirement.
A minimal erythema dose (MED) is the amount of UV radiation that will produce minimal erythema (sunburn or redness caused by engorgement of capillaries) of an individual’s skin within a few hours following exposure. http://www.ncbi.nlm.
It is well documented that excessive exposure to sunlight will increase risk of nonmelanoma skin cancers. However, it is also known that occupational sun exposure decreases the risk of melanoma, the most deadly form of skin cancer.
People of color who live near the equator and are exposed to sunlight on a daily basis sustain blood levels of 25(OH)D of 40-60 ng/ml. Their skin was designed to produce an adequate amount of vitamin D and the melanin pigmentation prevents the damaging effects minimizing risk of nonmelanoma skin cancer. A study in people who frequent a tanning bed at least once a week at the end of the winter had robust levels of 25(OH)D of approximately 40-50 ng/ml which was comparable to people of darker color being exposed to sunlight on almost a daily basis living near the equator. This is just a comparison; it is not to recommending you to go out and start using tanning bed every day!
As we age, our level of 7-dehydrocholesterol in skin will decrease. As a result, a 70 year old person has about 25% of the capacity to produce vitamin D3 in their skin compared to a young adult. However, because the skin has such a large capacity to produce vitamin D3, elders exposed to either sunlight, a tanning bed, or other UVB emitting devices are able to raise their blood levels of 25(OH)D often above 30 ng/ml.
How long a person should be exposed to sunlight to satisfy their vitamin D requirement? It depends on time of day, season of year, latitude, weather conditions and the person’s skin pigmentation.
Typically for a Caucasians skin in June at 46 degree latitude (at noon-time, exposure of arms and leg to sunlight on a clear day between the hours of 10 am and 3 pm for approximately 5-15 minutes, two to three times a week is adequate to satisfy the body’s vitamin D requirement. We should always use sun protection on our face since it is often the face that is most sun exposed and sun damaged. Our facial skin is much more delicate compare to our trunks’. After the 5-15 minutes of sun exposure, the application of a sunscreen with a SPF of at least 15 is then recommended if the you stays outside for a longer period of time in order to prevent sun burning and the damaging effects due to excessive exposure to sunlight.
Most experts agree that at least 800-1,000 lU of vitamin D/day is needed for all children and adults to help sustain healthy blood levels of 25(OH)D of >30 ng/mL. It is very difficult if not impossible to obtain this amount of vitamin D from dietary sources. It is also unrealistic to recommend that everyone on the planet increase their vitamin D intake to 1,000 lU of vitamin D/day and to avoid all direct sun exposure. Diet provides about 250-300 international units (lU) of vitamin D per day in the United States, primarily from vitamin D3-fortified foods such as dairy. A glass of fortified milk, though generally perceived as being a good source of vitamin D contains only 100 lU vitamin D, whereas being exposed to enough UVB radiation to cause a slight pinkness to the skin with most of the skin uncovered (1 minimal erythemal dose) produces vitamin D equivalent to an oral dose of 20,000 lU vitamin D. On the other hand, in higher latitudes during the winter months no vitamin D is made from sun exposure so diets and supplements become relatively more important sources. One important issue is that ergocalciferol (D2) is often used in supplements and ergocalciferol has been estimated to be only one-fourth as potent as cholecalciferol (D3) in raising 25(OH)D.
The risk of skin cancer should generally be of much less concern than the health benefits of vitamin D for most people. The analysis of the economic burden of solar UVB irradiance and vitamin D deficiencies compared to excess solar UV irradiance for the United States yielded interesting findings. One was that the US economic burden due to vitamin D insufficiency from inadequate exposure to solar UVB irradiance, diet and supplements was estimated at $40 billion to $56 billion in 2004, whereas the economic burden for excess UV irradiance was estimated at $6 billion to $7 billion. These findings are probably still approximately correct, if not on the low side, with respect to vitamin D because of the additional benefits found recently, such as protection against infectious diseases.
Recent evidence suggests that higher vitamin D intakes beyond current recommendations may be associated with better health outcomes. The most advantageous serum levels for 25(OH)D appeared to be at least 75 nmol/L (30 ng/ml) and for cancer prevention, desirable 25(OH)D levels are between 90-120 nmol/L (36-48 ng/ml). An intake of no less than 1000 lU of vitamin D3 (cholecalciferol) per day for all adults may bring at least 50% of the population up to 75 nmol/L (30 ng/ml). Thus, higher doses of vitamin D are needed to bring most individuals into the desired range. Based on bone mineral density study in younger and older adults it is suggest that serum 25(OH)D levels of at least 75 nmol/L (30 ng/ml) are desirable. The result that you see on your total vitamin D test from your doctor will most likely in (ng/ml) unit. So shoot for a number above 30 on your test result 😀
The bottom line: I’m not suggest you start go sunbathing or tanning. What I’m trying to tell you is that the sun is not harmful as it has been portray for many years. I’m here to provide information so you can be more inform and make your own decision. Base on all the info I found that the benefit is outweigh the risk of getting skin cancer. The amount of time need to spend in the sun to make enough vitamin D won’t get you burn 🙂 I’m willing to take a walk outside for 5-15 min. during 10am-3pm twice a week to get my dose of vitamin D…Always wear sunscreen on your face & hand (since the first sign of aging will appear there!) and a hat would be even better! Also after the 5 min remember to apply sunscreen if you stay outside longer.
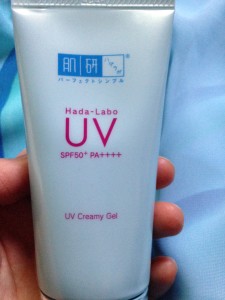
My current sunscreen is Hada-Labo UV Creamy Gel SPF 50/PA ++++. I tried many sunscreen before but this by far my favorite. And I know it does contain alcohol but it’s very gentle, it doesn’t dry out or irritate my skin. Best of all it really help control my sebum. Normally my T-zone is very oily but this sunscreen help control it and really reduce the blackheads on my nose! Kerry wrote a really detail review about it here. I order mine from Amazon for $10.88
Here’s my gear when out in the sun:

Can’t forget my wide-brimmed hat! I like coolibar hat and Tula hat.
and my coolibar shirt (I wear long sleeves when I don’t need my dose of vitamin D)

Sources:
Understand UVA and UVB http://www.skincancer.org/
Minimal Erythema Dose (MED) testing http://www.ncbi.nlm.
Book: Skin cancer-A practical approach
Book: Sunlight, Vitamin D, and Skin cancer
PDF article: Diversity of Biological Effects induced by Longwave UVA Rays (UVA1) in reconstructed skin